Osseointegration and Dental Implants: A Comprehensive Guide
In the evolving field of dentistry, the term “osseointegration” has emerged as a cornerstone concept, particularly in the context of dental implants. This article aims to demystify osseointegration, explaining its significance, process, duration, potential challenges, and the role of bone grafting in ensuring successful dental implantation.
Dental Implant Surface and Osseointegration
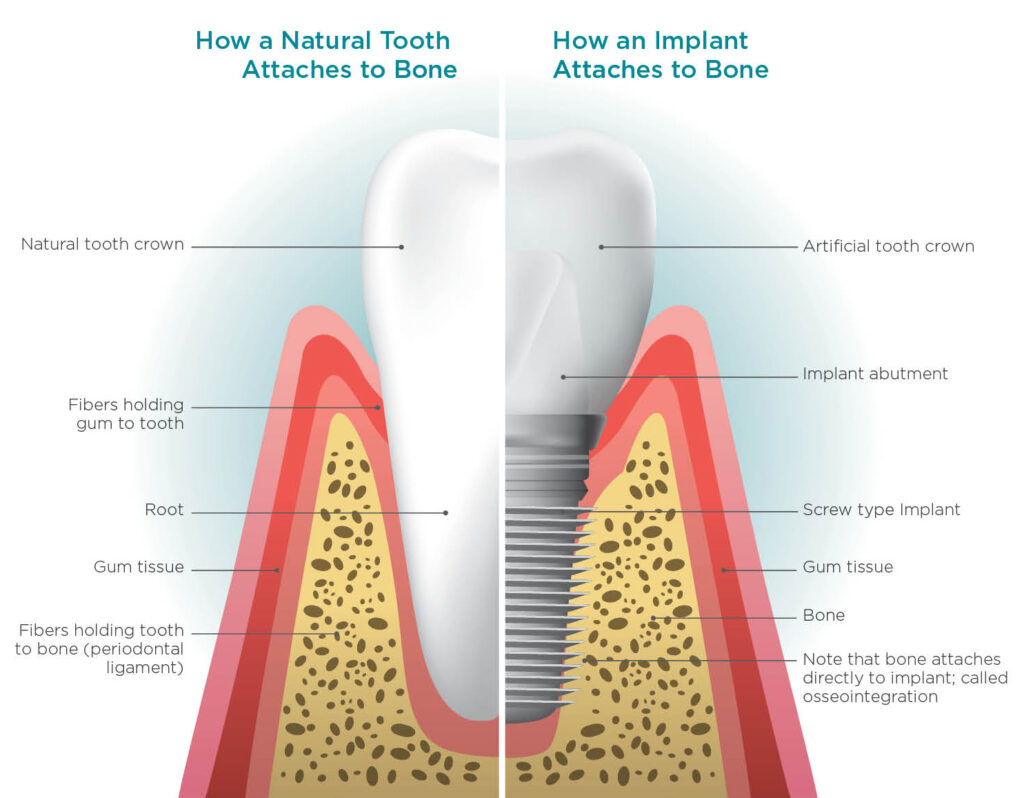
To understand osseointegration and its relation to dental implants, you need to know that a dental implant consists of three parts: the implant fixture, the abutment, and the crown. Osseointegration is related to the implant fixture stage.
The Implant Fixture
This small, screw-like structure is usually made of titanium and surgically placed into the jawbone. It acts as a synthetic tooth root, providing a sturdy foundation for the artificial tooth. Like a natural tooth root, the fixture is the solid base upon which the rest of the dental implant system is built, so understandably, it must be very strong and set in place.
The Abutment
Situated above the gum line, the abutment connects the implant post to the crown. It’s a crucial component that ensures the stability of the entire structure.
The Crown
This is the visible part of the implant, usually made of ceramic or porcelain, designed to mimic the appearance and function of a natural tooth.
The Process
The process of getting dental implants involves several steps:
- Implant Placement: Surgical insertion of the implant post into the jawbone.
- Healing and Osseointegration: A period for the implant to integrate with the bone, usually taking several months.
- Abutment Placement: Once healing is complete, the abutment is attached.
- Crown Fitting: The custom-made crown is placed on the abutment.
What is Osseointegration?
Osseointegration is a biological process where a dental implant fixture, typically made of titanium implant or a metal-free ceramic, forms a direct bond with intervening soft tissue of the jawbone. This integration is crucial for the stability and longevity of the implant. This allows the dental implant fixture to act like the natural tooth root.
A Historical Perspective
Swedish Orthopaedic Surgeon Per-Ingvar Brånemark (3 May 1929 – 30 December 2014) is known as “the father of modern dental implantology”. He discovered the concept of osseointegration in the 1950s and observed the structural and functional connection that titanium could bond irreversibly with living bone tissue. This finding revolutionised osseointegration surgery and implant dentistry to this day.
How Osseointegration Works with Dental Implants
With the implant procedure, the implant fixture is placed into the jawbone; the body initiates a healing process where new bone cells attach directly to the titanium implant surface, essentially “locking” the metal implant into the jawbone, producing osseointegrated dental implants.
The Process
- Implant Placement: The titanium implants are surgically inserted into the jawbone.
- Healing Phase: The soft tissue and bone grow around the implant.
- Osseointegration: The implant bonds to be part of the natural jawbone (over time).
Timeline for Osseointegration
The duration or ‘the how long’ of osseointegration varies but typically ranges from 3 to 6 months. Factors influencing this timeline include:
- The health and density of the patient’s bone.
- The location of the implant.
- The type of implant used.
Is Osseointegration Painful?
Osseointegration to the implant surface is when the dental implant fuses with the jawbone’s soft tissues and is not painful. This is because the connective tissue process occurs gradually over months, and there are no nerve endings in the bone to transmit pain sensations.
However, there are levels of discomfort experienced as part of your surgical journey and vary depending on several factors:
- Surgical Procedure: The initial implant surgery might cause discomfort. Post-surgical pain is usually manageable with over-the-counter pain relievers or prescribed medications. Most patients report less discomfort than expected, often comparing it to a tooth extraction.
- Individual Pain Threshold: Pain tolerance varies from person to person. A mild discomfort for one individual could be more painful for another. Honest communication between you and your Aria dentist is important; they are there to help you.
- Post-Operative Care: Proper care after the surgery can greatly impact the level of discomfort. Following your Aria dentist’s instructions regarding oral hygiene, diet, and medication is crucial.
- Healing Complications: If any complications arise during the healing process, such as infection or inflammation, this could cause additional discomfort. It’s essential to monitor the healing process and consult your Aria dentist if there are signs of complications.
- Immediate vs. Delayed Loading: The approach taken (immediately placing a crown on the implant vs. waiting for the bone to heal first) can influence discomfort during the osseointegration period.
While the surgery and the healing process may involve some discomfort, the process of osseointegration itself is not painful. With modern surgical techniques and proper post-operative care, most patients find dental implant surgery and recovery less discomfort than anticipated. It’s always advisable to discuss any concerns about pain with the dental surgeon before the procedure.

What if Osseointegration Fails?
The failure of osseointegrated titanium implants can result in the loosening or rejection of the implant. Your implants should not be able to move or cause you discomfort.
The failure rate of dental implants is relatively low. Still, it can vary depending on various factors, including the patient’s oral health, lifestyle, and the skill and experience of the dental professional performing the implant procedure itself.
Medical studies report that dental implant failure rates happen to less than 5% of patients. Dental implants are a successful long-term solution for most patients for replacing missing teeth.
Osseointegration or implant failure causes include:
- Patient-Specific Factors: Conditions like diabetes, osteoporosis, or habits like smoking can significantly increase the risk of osseointegration failure. Poor oral hygiene and certain medications might also affect implant success.
- Quality and Quantity of Bone: Adequate bone density and volume are crucial for implant stability. Patients with insufficient bone mass, which might require bone grafting to allow for osseointegration to the implant surface, can have higher failure rates.
- Location of the Implant: Titanium implants in the back of the mouth (molars) have a slightly higher failure rate than those in the front, possibly due to the higher bite forces in these areas.
- Surgical Technique and Implant Quality: The dental surgeon’s expertise and the implant’s quality are also critical factors. Advanced surgical techniques and high-quality implants tend to have lower osseointegration failure rates.
- Immediate Loading of Implants: Implants loaded with a tooth replacement (like a crown) immediately after surgery might have a higher risk of failure, particularly in areas where poor bone quality and excessive pressure interrupt the osseointegration.
- Periodontal Disease: Patients with a history of periodontal (gum) disease may have a higher risk of osseointegration and implant failure due to the potential for inflammation and infection around the implant site.
In such osseointegration failure cases, the implant may need to be removed, and the area allowed to heal before attempting re-implantation.
Connective Tissue: The Role of Bone Grafting in Osseointegration
Bone grafting is used to augment the quantity and quality of bone inside the jaw’s soft tissue. The lack of or poor bone tissue is a direct structural and functional issue for oral implants. Bone grafting improves bone regeneration in the surrounding bone tissue and the chances of osseointegrated implants.
When is Bone Grafting Needed?
- Insufficient bone density or volume, which won’t allow for osseointegration.
- Bone loss due to periodontal disease or tooth loss.
- Enhancing the success rate of osseointegration in challenging cases.
Types of Bone Implant Interface
- Autografts: Bone harvested from the patient’s own body.
- Allografts: Bone sourced from a human donor.
- Xenografts: Bone derived from animal sources.
- Synthetic Materials: Biocompatible, artificial substances.
Post-Operative Care and Maintenance
After dental implant surgery, proper post-operative care is crucial for successful healing and osseointegration. This period, typically lasting several months, requires meticulous attention to oral hygiene and lifestyle habits during the implant integration with the jawbone.
Here’s a comprehensive care guide:
Immediate Post-Operative Care
- Pain Management: Use prescribed painkillers or recommended over-the-counter medication to manage discomfort.
- Swelling Reduction: Apply cold packs to the cheek area intermittently (20 minutes on, 20 minutes off) for the first 24-48 hours.
- Bleeding Control: Bite gently on a gauze pad and change as needed. Minimal bleeding is normal.
Oral Hygiene
- Gentle Cleaning: Brush teeth gently, but avoid the surgical site for the first few days. Gradually clean the area around the dental implants with soft brushes.
- Mouth Rinses: Use saltwater rinses or prescribed antimicrobial mouthwashes to reduce bacterial buildup.
- Avoiding Irritation: Refrain from using straws, smoking, or consuming hot and spicy foods that might irritate the surgical site.
Diet and Nutrition
- Soft Diet: Stick to soft foods like yogurt, soup, and applesauce for the first few days. Gradually reintroduce solid foods as comfort allows.
- Hydration: Stay well-hydrated with water or non-acidic juices.
- Nutrition: Maintain a balanced diet to support healing.
Activity and Lifestyle
- Rest: Limit physical activity for the first 24-48 hours to minimise swelling and bleeding
- Smoking: Smoking can impair healing and osseointegration.
- Alcohol: Refrain from alcohol consumption, as it can interfere with the healing process.
Regular Dental Check-ups
- Follow-up Visits: Attend all scheduled post-operative appointments to monitor the healing process and osseointegration.
- Professional Cleanings: Regular dental cleanings and check-ups are vital for maintaining implant health.
Monitoring for Complications
- Infection Signs: Watch for signs of infection, such as persistent pain, swelling, or unusual discharge.
- Loosening or Discomfort: Report any loosening or discomfort around the implant to your dentist.
Long-Term Care and Maintenance
- Oral Hygiene Routine: Continue with regular brushing and flossing.
- Professional Monitoring: Ongoing dental check-ups to monitor the implant’s and surrounding tissues’ health.
The success of dental implants heavily depends on the care taken during the first wound healing and osseointegration phase. By following these guidelines, patients can significantly enhance the outcome of their implant surgery. Always remember that individual recommendations may vary based on the patient’s health and the specific circumstances of the surgery, so it’s essential to follow the advice provided by your dental surgeon or dentist.
Need more Osseointegration Information? Aria can help.
Osseointegration is a fascinating and intricate process at the heart of modern dental implantology. Understanding its principles, challenges, and the supportive role of procedures like bone grafting can significantly impact the success of dental implants, offering patients a durable and functional solution to tooth loss.
As dental technology advances, the scope of osseointegration continues to expand, paving the way for more effective and patient-friendly dental restoration techniques. If you are considering dental implants, you need to consult with our Aria Dental professionals to understand your specific needs and suitability for dental implants, ensuring the best outcomes in your oral health journey.
To book a free dental implant consultation with your choice of Aria Dental dentist and locations – contact our Patient Services team on 08 9226 2135.
